Sign up to our newsletter!
Fibromyalgia
Fibromyalgia is a real disease and can be treated. Here is how I diagnose and treat patients with this condition.
 Young lady with chronic pain, fatigue and brain fog from fibromyalgia.
Young lady with chronic pain, fatigue and brain fog from fibromyalgia.Fibromyalgia is a real disease. 20 years ago, many doctors too did not believe that fibromyalgia exists. Now, most do.
Fibromyalgia is a condition that causes fatigue, chronic pain at multiple spots, joints, muscles and tendons as well as brain fog in sufferers, believed to be due to damages to the nerve and muscle structures from abnormal sleep patterns.
There may be associated long term depression and other psychiatric issues.
Women are 6 times more affected than men are.
Because people who suffer with this condition look well and there is no blood test or “x-rays” that can be done to confirm the diagnosis, family members and healthcare providers may take a long time to come to appreciate that you suffer with this condition.
Many people who suffer from this condition often remember when they were once well, then they came down with a very bad flu, or severely stressful situation, prolonged anxiety, injury, etc, and they never recovered.
Fibromyalgia is NOT an autoimmune disease or an inflammatory disorder.
Typical symptoms of Fibromyalgia include:
- Chronic pain at multiple points - muscles, joints, of more than 3 months duration. Once not too long ago, doctors used to depend on the presence of 11 out of 18 tender spots before making a diagnosis of fibromyalgia. That criteria has gone the way of the dodo, horse and buggy.
- Difficulty with having restful sleep. Though many experts believe that this is the origin of this condition, it is a very common symptom of fibromyalgia - waking up and not feeling rested. Many patients with fibromyalgia also struggle to go to sleep and stay asleep.
- Difficulty with memory, concentration and decision making. This is also referred to as a fibro fog or brain fog. I think the picture of the December 5th to 9th 1952 London fog is a perfect description of what many of my patients describe. They can remember or think about things, but their mind is only as clear as looking through the skies of London during the smog.
- Chronic fatigue. This is a different type of tiredness - one that does not go away yet, made worse my doing anything. The other day, I had a 54 year old gentleman with fibromyalgia who told me that even if he clears snow from his driveway, it would take him another two days to recover from the fatigue and pain that ensues. Activity makes this fatigue worse and that is one of the biggest problem to overcome in treatment because exercising (graded exercise) is part of the treatment regimen.
- Hypersensitivity to light, sounds, perfumes and more. This is another common but not well understood or even acknowledged component of fibromyalgia syndrome. Patient J is a gentleman in his early 60s with fibromyalgia, but debilitated more by the fact that he cannot attend his regular weekly meetings with friends. He is easily irritated by scents, changes in the weather, cold and light. These triggers do not only cause him emotional distress, but worsens his chronic pain and fatigue.
- Concomitant presence of irritable bowel syndrome and or depression. This is why some doctors struggled with the notion that fibromyalgia is not a mental health problem. No, it is not. It is a rheumatologic-psychiatric issue. The primary cause rests with distortion of how brain, nerves and muscles responds to stimuli and information processing and transmission. Those with fibromyalgia often have irritable bowel syndrome (IBS) - chronic abdominal pain, bloating, constipation and or diarrhea, exacerbated by certain foods or stress. IBS is believed to reflect the general brain and nervous system hypersensitivity triggered by the cause of fibromyalgia. Depression in this condition is difficult to explain, but may well be due to a response to the debilitating nature of this condition, lack of understanding and empathy from close friends and family members and isolation as well as job loss, economic difficulties and reduced overall quality of life experienced.
The diagnosis of fibromyalgia is wholly based on the symptoms and examination findings of your doctor. You do not need a rheumatologist to diagnose fibromyalgia. I have a specialist interest in chronic pain management and has been diagnosing and treating patients with fibromyalgia for many many years.
Before making a diagnosis of fibromyalgia, it is often helpful to exclude conditions that can be mistaken for fibromyalgia. These include:
- Chronic fatigue syndrome
- Lupus
- Arthritis
- Polymyalgia rheumatica
- Under-functioning thyroid gland (hypothyroidism)
- Hyperthyroidism
- Low testosterone syndrome (hypogonadism)
- Anemia
- Multiple sclerosis (MS)
- Lyme disease
- Adrenal gland disease.
This can be done with a single comprehensive blood panel in most cases, but for the presence of MS which requires more investigations. I do not routinely screen my fibromyalgia patients for MS, as the history tends to help in most cases.
So, how is fibromyalgia treated?
I always follow a structured approach to treating my patients with fibromyalgia. The steps I take include:
- Collaboratively walking my patients through their symptoms and examination findings and help them to come to make the diagnosis by themself or why I strongly believe that this is what they have. I call this process establishing diagnostic concordance. It may involve reviewing more recent evidence, help them discard obsolete diagnostic criteria and creating that clarity for their personal situation. I find that this step is very important even in those patients who already suspects or know that this is their diagnosis. It helps my patients and I to be on the same page both in terms of diagnosis, treatment and management of this complex life-consuming condition. It also helps me to drive it into my patients consciousness that this illness is real, is not their fault, they should not feel frustrated that they are not understood by their family, friends and healthcare providers, but that it is completely manageable.
- Once we have done the above, I ask my patients to write out what they believe is the most pressing or distressing symptom for them. No. Not symptoms. It is important to tease out what is more of a problem - is it the fatigue, or pain or environmental sensitivity or fibro fog. I ask them to score that on a scale of 1 to 10, 10 being the most severe grade this symptom could be. Once we isolate what matters most to them, I also ask that the other symptoms are scored, using the same visual analogue system of 1 to 10. This is to help us establish the current level of debilitation, define expectations, create well defined treatment goals, as well as gauge outcome on a mutually agreed horizontal metric.
- Discuss available non-drug and drug treatment approaches available for fibromyalgia and assess their initial preferences and belief systems in relationship to treatment choices. This is to establish their therapeutic preference and identify very early, possible problems with compliance with prescriptions. many patients with fibromyalgia are fed up with trying different medications and failures by the time their diagnosis is made. They might have lost faith in the healthcare system because they might have been told all along that their symptoms is all in their head or mind.
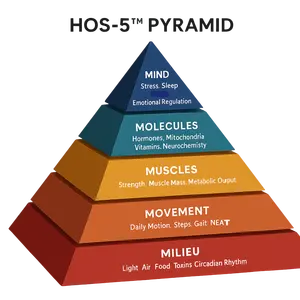
- Getting patients back to the basics and work to get to the root of the problem. This is where the different between succeeding or not lies. Doctors generally do less of this these days because of how our healthcare system functions. Success with treatment of fibromyalgia comes from re-establishing the pre-illness condition of the patient, by working through in great details, the sleeping, eating, exercise and relaxation rituals and habits of patients. Yes. I could be really petty here. I want to know what you do in the preceding 4 hours before bed, when you go to bed, how your bedroom is set up, what is the average temperature of your room, do you read or work from your bedroom, do you have TV or computer in your bedroom, what type of bed and mattress do you sleep with and for how long now have you had the mattress, what about your pillow type, are you a side sleeper or sleeps best on your abdomen or back, do you snore, if you do, have you been tested for obstructive sleep apnea, do you suffer with arthritis or other joint problems, how long it takes you to actually sleep off, how long you stay asleep, what wakes you up, how long you stay awake before you go back to sleep if you do eventually go back to sleep, if you are on sleeping pills and which type and dose, for how long have you been taking the sleeping pill for, when do you wake up finally, what do you do once you wake up in the morning (your morning routines), do you find yourself sleepy in the daytime, needing naps? How long do you nap for. I do the same for your foods and drinks, recreation, exercise, relaxation, relationships and then we work together to optimise things where necessary. I often find that when these basic physiologies are well optimised, symptoms are cut down by at least 30 percent within the first 3 months.
- Graded Exercise. Ah ha. I know what you are thinking. How can I exercise when it burns me out. Well, you can and it is one of the most powerful things you can do to get you back on the road to recovery. Studies show that being able to establish and stick to a graded or graduated exercise program will cut off another 30% of your pain. So what is graded exercise. It means starting and working out in small increments. I start my patients with a 5 minutes walk around the block every day for the first two weeks, then increase this to 10 minutes walk daily. If they feel too exhausted by that increment, we cut it down to 7 minutes until they get used to that and we gradually increase this every two weeks to three weeks until they can walk for 20 to 60 minutes every day. We then include small strength building exercises and do the same. In fibromyalgia, as in good health, I remind my patients that to hurt while doing exercises does not mean you are doing damage to your body. As long as you take time to allow recovery, you get stronger and better.
- Drugs. Off course. There are drugs that helps with the control of fibromyalgia. If my patient tells me that sleep is their biggest problem, I start with melatonin and amitriptyline. Melatonin is to help restore the circadian cycle or natural sleep pattern, supported with optimal sleep hygiene, lifestyle and behavioural changes. Amitriptyline also helps with sleep and chronic pain sensation. Other drugs used in fibromyalgia include gabapentin, antidepressants, muscle relaxants and IBS meds. I adapt my prescriptions to match your specific most pressing symptoms and work to control that.
- Cognitive Behavioral Therapy (CBT). I cannot stress enough the benefit of CBT in the hands of very experienced CBT practitioners. Medical evidence abounds that shows that dealing with the “internal worries” and “meaning” of life helps improve sleep, pain sensation, mood, and overall quality of life. Closely linked to CBT is neuro linguistic programing, NLP. I offer NLP based therapy to selected patients. CBT and NLP, in my experience are superior to the traditional psychoanalytic old school psychotherapy approach in dealing with fibromyalgia.
If you suffer with a combination of the above symptoms and now belief or even still in doubt that you have fibromyalgia, speak to your doctor and get referral to a physician with interest and experience in dealing with this condition or a rheumatologist and get help.
Fibromyalgia is treatable. Don’t suffer in silence.
Stay Connected




New! Comments
Have your say about what you just read! Leave me a comment in the box below.